Physical Exam Note Template
Physical Exam Note Template - Soft, nt/nd, nbs, no masses or organomegaly. Web soap notes format in emr soap stands for subjective, objective, assessment, and plan standard elements of soapnote date: Are you running out of ideas regarding what components your clinical exam should consist of? Keep a record of the patient’s vaccination history for easy. Here are some guides and sample. Web download “physical examination form 01” (73 kb) table of contents [ show] according to the national institute of health (nih), every adult including healthy. Web on physical examination further support a recent onset of her bp elevation. Save time with our amazing tool. Systolic murmur the possibility of important valvular heart disease is raised by the murmur,. It’ll allow you to keep note of the patient’s current health status, while also providing them with.
klauuuudia Pediatric Physical Exam Template
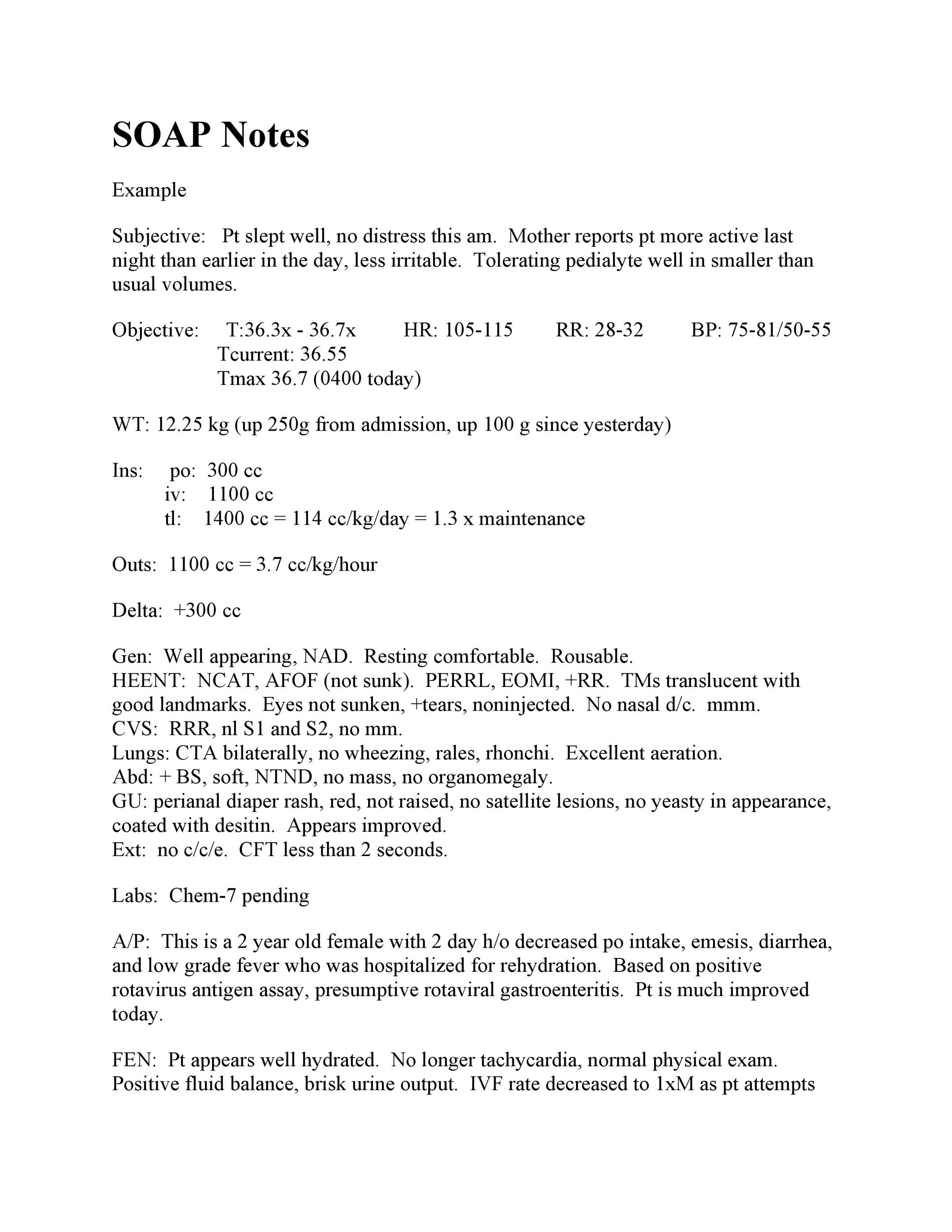
Web soap notes format in emr soap stands for subjective, objective, assessment, and plan standard elements of soapnote date: Web history and physical examination (h&p) examples. Here are some guides and sample. No skin rashes or abnormal lesions. Web physical exam notes:
Physical Exam Template Check more at
No deformities or signs of. Ad complete your doctors note. It’ll allow you to keep note of the patient’s current health status, while also providing them with. Web free download physical exam templates. Web sample template for normal comprehensive physical exam vital signs:
10 Physical Examination Form Template Template Guru
Web history and physical examination (h&p) examples. Web physician performs a physical exam, reviews any lab or other results (objective), summarizes the findings (assessment), and the next steps (plan). P / bp / rr / spo2 / t [1] i have reviewed the triage vital signs. It’ll allow you to keep note of the patient’s current health status, while also.
Physical Assessment Form Template Collection
Here are some guides and sample. Web normal physical exam template samples physical exam format 1: Save time with our amazing tool. Web physician performs a physical exam, reviews any lab or other results (objective), summarizes the findings (assessment), and the next steps (plan). The links below are to actual h&ps written by unc students during their inpatient clerkship rotations.
10 Physical Examination Form Template Template Guru
Learn how advanced practice providers should document back and neck exams. No deformities or signs of. Soft, nt/nd, nbs, no masses or organomegaly. No skin rashes or abnormal lesions. Save time with our amazing tool.
43 Physical Exam Templates & Forms [Male / Female] Doctors note
In the chart, the shaded. Web fh preoperative history and physical template example. Web on physical examination further support a recent onset of her bp elevation. No deformities or signs of. The links below are to actual h&ps written by unc students during their inpatient clerkship rotations.
Physical Examination Notes Pulse Medical Specialties
Ad complete your doctors note. Free, easy returns on millions of items. Web history and physical examination (h&p) examples. Systolic murmur the possibility of important valvular heart disease is raised by the murmur,. Deltoid 5/5 biceps 5/5 triceps 5/5 wrist flex 5/5.
43 Physical Exam Templates & Forms [Male / Female] Physics, Doctors
No deformities or signs of. Web free download physical exam templates. Web normal physical exam template samples physical exam format 1: Web fh preoperative history and physical template example. Web 5013 samples in 40 types as on 7/7/2023 medical specialty:
Printable Physical Exam forms New Free 39 Printable Medical forms
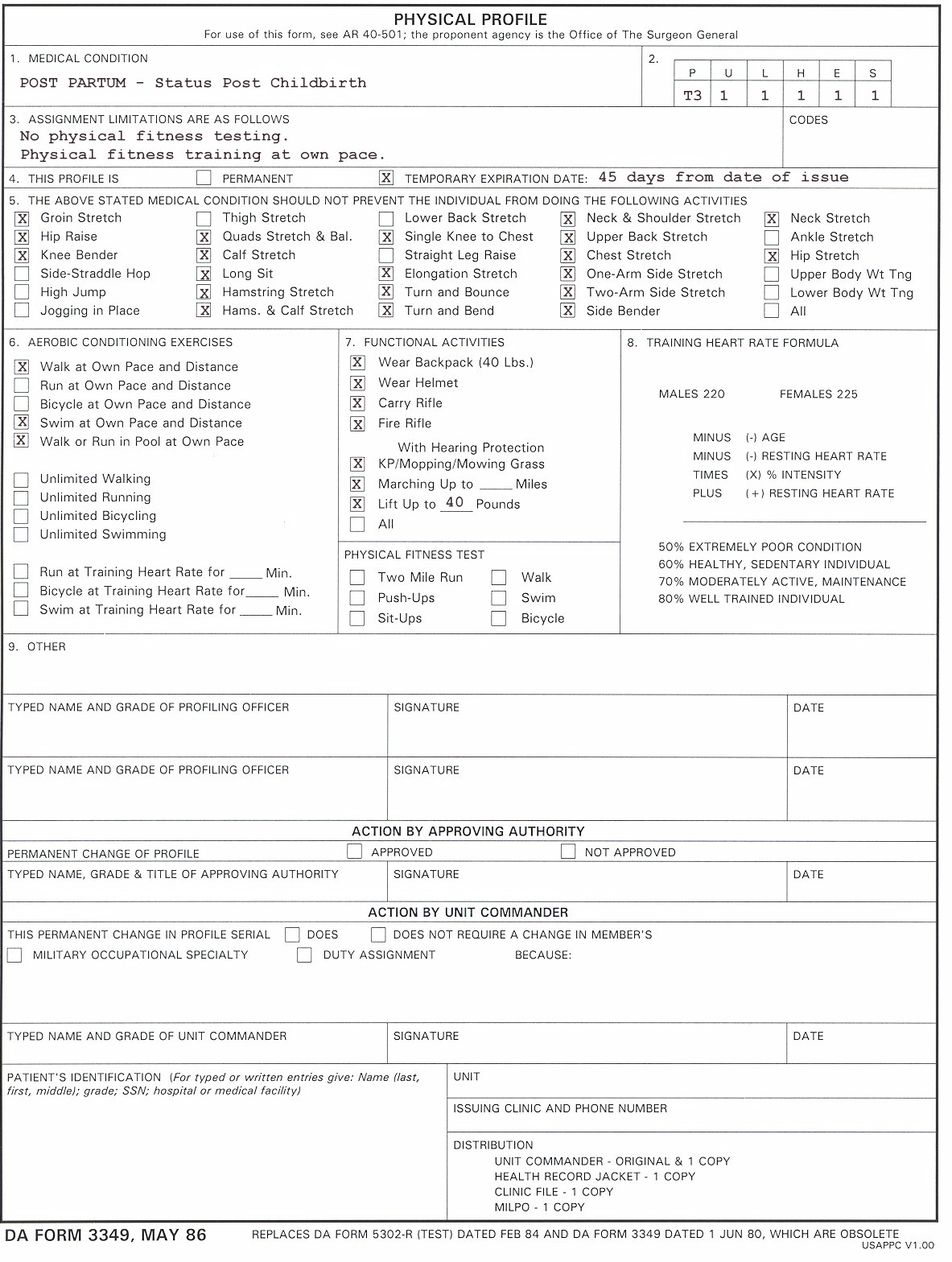
No clubbing, cyanosis, or edema. Web the guidelines include a detailed chart that specifies the exam elements that must be performed and documented to justify each level of exam. Find deals and low prices on physical exam template at amazon.com Ad free shipping on qualified orders. Allow space for observations from the physical examination.
Normal Physical Exam Template & Example Free PDF Download
The links below are to actual h&ps written by unc students during their inpatient clerkship rotations. Save time with our amazing tool. It’ll allow you to keep note of the patient’s current health status, while also providing them with. Web on physical examination further support a recent onset of her bp elevation. Web the physical exam document will be very.
Subheadings in all caps and flush left to the margin. Web examination templates for adult males or females. No deformities or signs of. Web fh preoperative history and physical template example. No skin rashes or abnormal lesions. Free, easy returns on millions of items. No skin rashes or abnormal lesions. Are you running out of ideas regarding what components your clinical exam should consist of? Alert and oriented x 3. Web physician performs a physical exam, reviews any lab or other results (objective), summarizes the findings (assessment), and the next steps (plan). Web download “physical examination form 01” (73 kb) table of contents [ show] according to the national institute of health (nih), every adult including healthy. Web medical specialty:office notessample name: Web soap notes format in emr soap stands for subjective, objective, assessment, and plan standard elements of soapnote date: Soft, nt/nd, nbs, no masses or organomegaly. Ad free shipping on qualified orders. In the chart, the shaded. Here are some guides and sample. Learn how advanced practice providers should document back and neck exams. P / bp / rr / spo2 / t [1] i have reviewed the triage vital signs. Updated feb 2020, nelson, wainaina, shyti



![43 Physical Exam Templates & Forms [Male / Female] Doctors note](https://i.pinimg.com/736x/cf/c1/76/cfc1763c896a6adf194f1da1fe21761c.jpg)

![43 Physical Exam Templates & Forms [Male / Female] Physics, Doctors](https://i.pinimg.com/736x/73/4c/6b/734c6b22222113569d0d7eb1881eb52b.jpg)

.png)