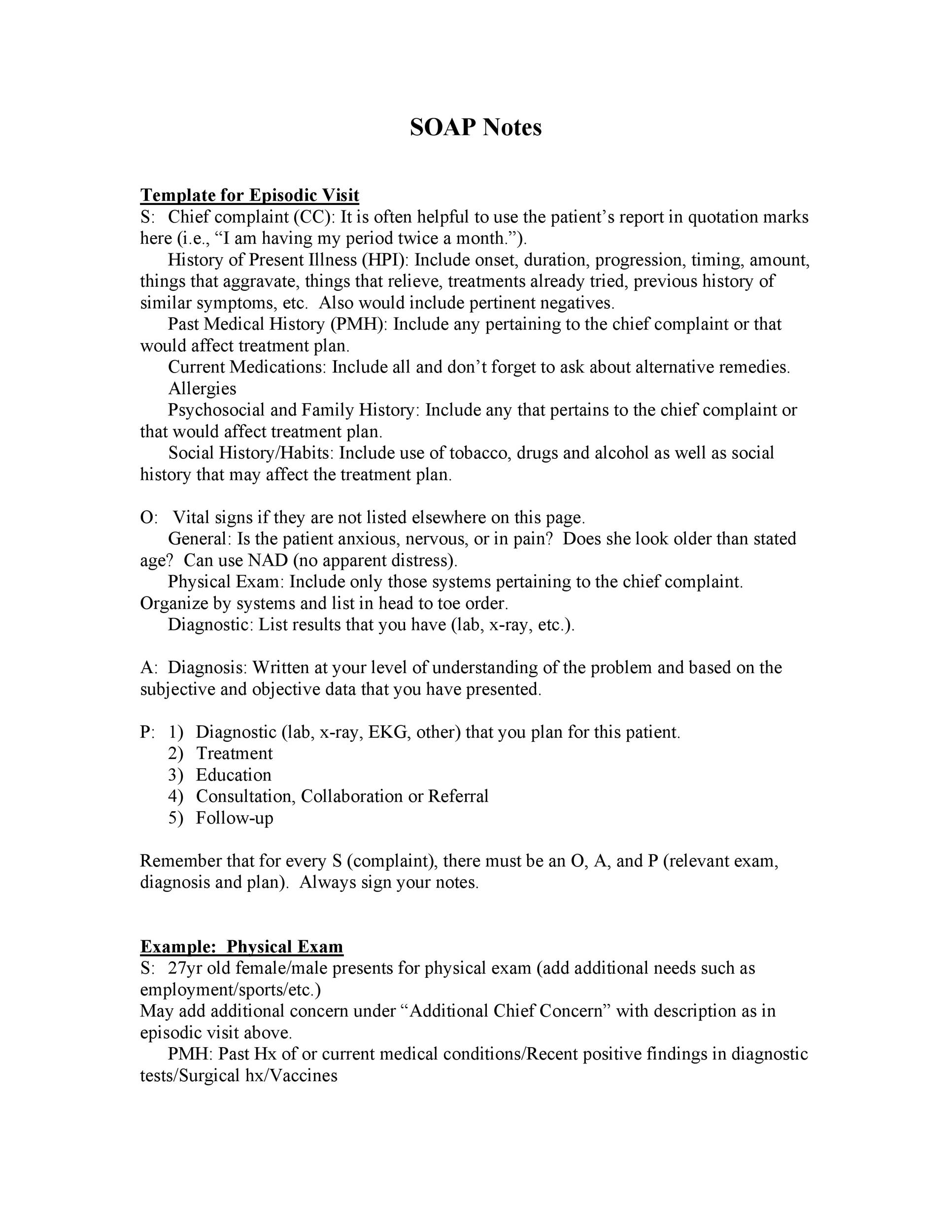
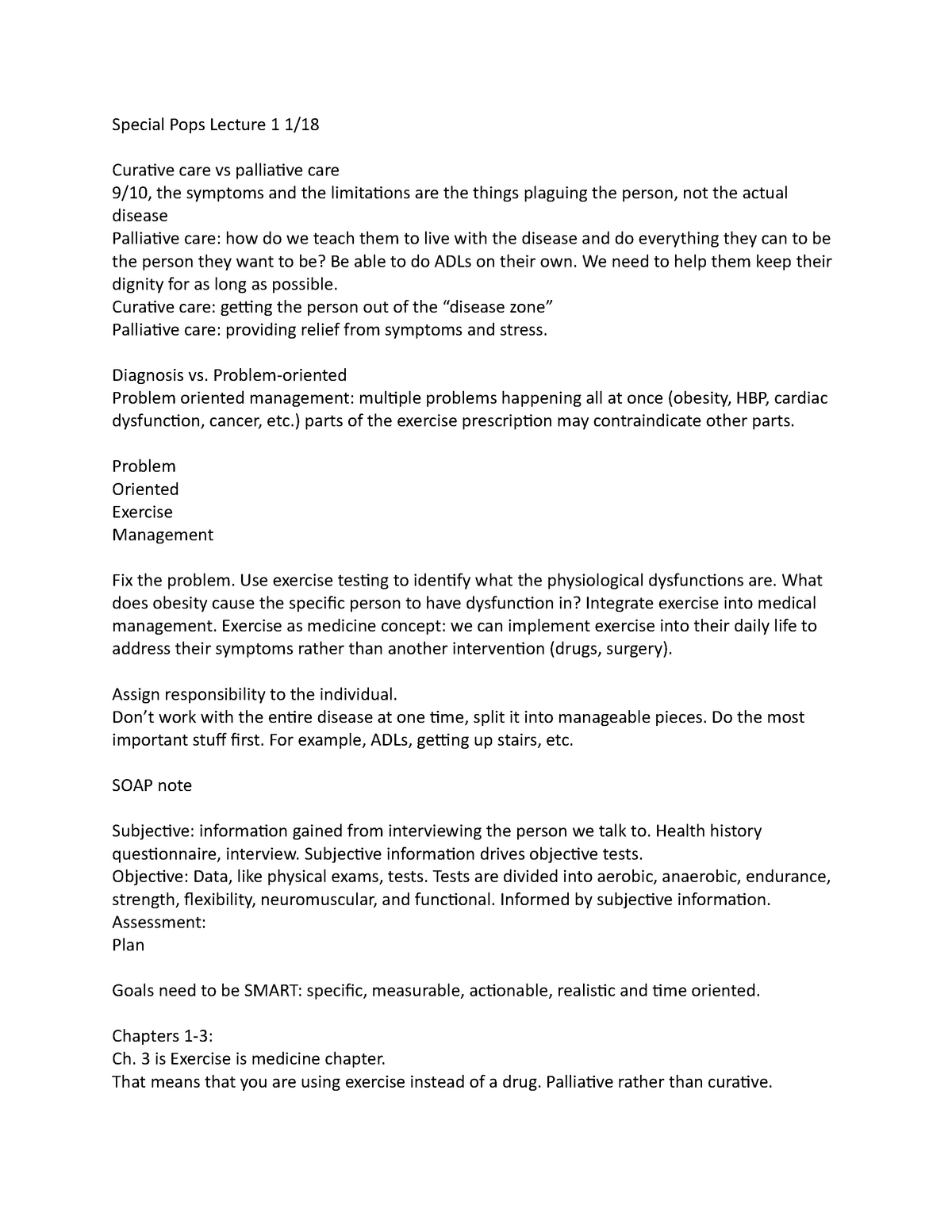
Physical Exam Template Soap Note
Physical Exam Template Soap Note - Well developed, well nourished, alert and cooperative, and appears to. Web a soap note is an acronym of subjective, objective, assessment and plan which represents a method of documenting a patient’s health record by the healthcare. Learn more from thriveap the leading virtual np transition to practice education. Detailed findings concerning the look, actions, physical expressions, and emotions of the patient could be. Web templates for issues that require secondary screening items can be easily integrated into the annual physical template with the soap note generator. Free, easy returns on millions of items. Web cite favorite 2 approximately 126 views in the last month. Web a soap note’s objective section contains realistic facts. Web the subjective, objective, assessment and plan (soap) note is an initials representing a widely used method of documentation for healthcare providers. Web updated february 3, 2023 subjective, objective, assessment and plan (soap) notes are used in physical therapy to record important details about a patient's.
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
Web physician performs a physical exam, reviews any lab or other results (objective), summarizes the findings (assessment), and the next steps (plan). Oral cavity and pharynx normal. Vital signs including oxygen saturation when indicated. Web original soap note usage guide. Web the subjective, objective, assessment and plan (soap) note is an initials representing a widely used method of documentation for.
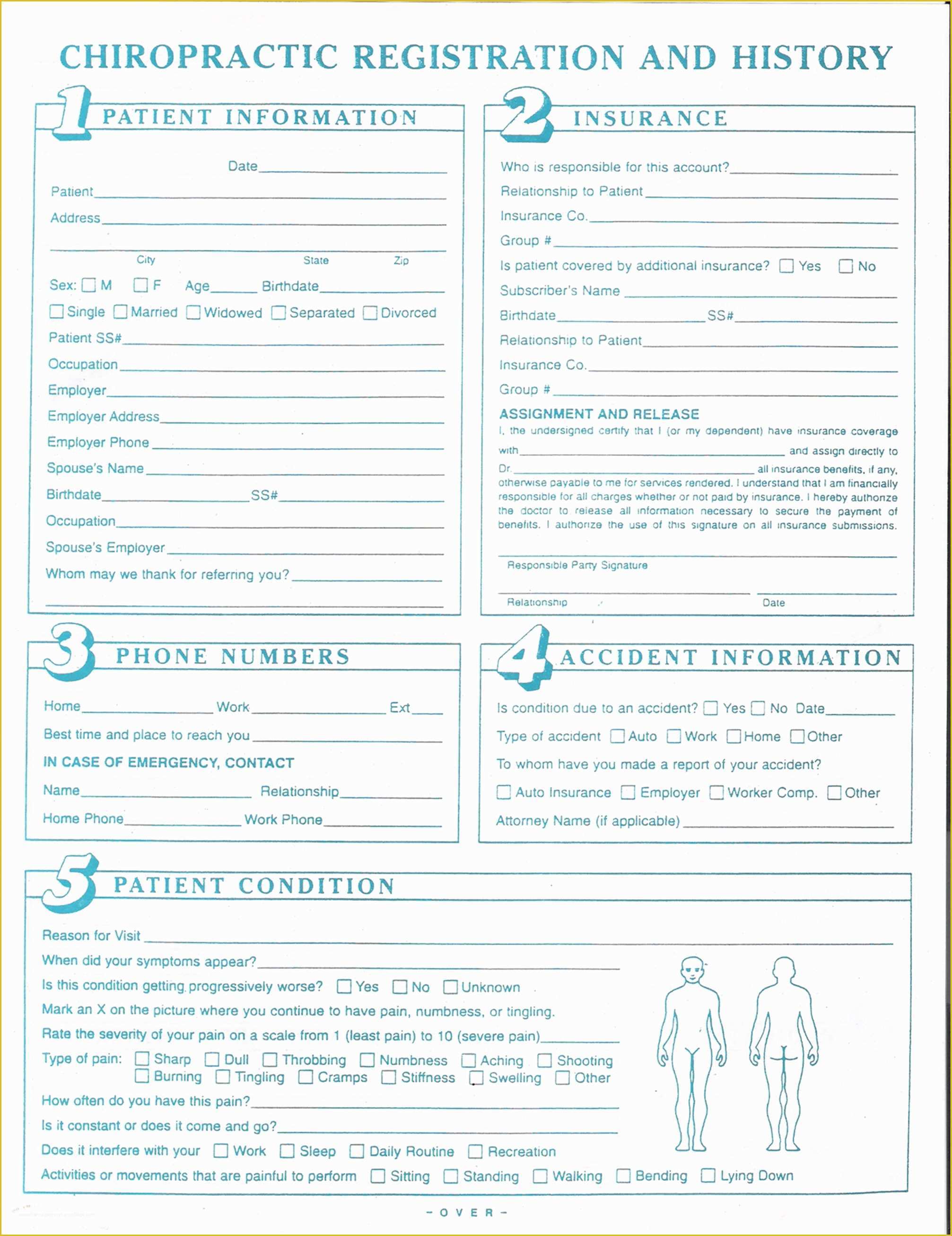
Chiropractic soap Notes Template Free Of Work Physical Exam Blank form
Web the subjective, objective, assessment and plan (soap) note is an initials representing a widely used method of documentation for healthcare providers. The soap note is a way. Web a soap note is an acronym of subjective, objective, assessment and plan which represents a method of documenting a patient’s health record by the healthcare. Web dry notes are the backbone.
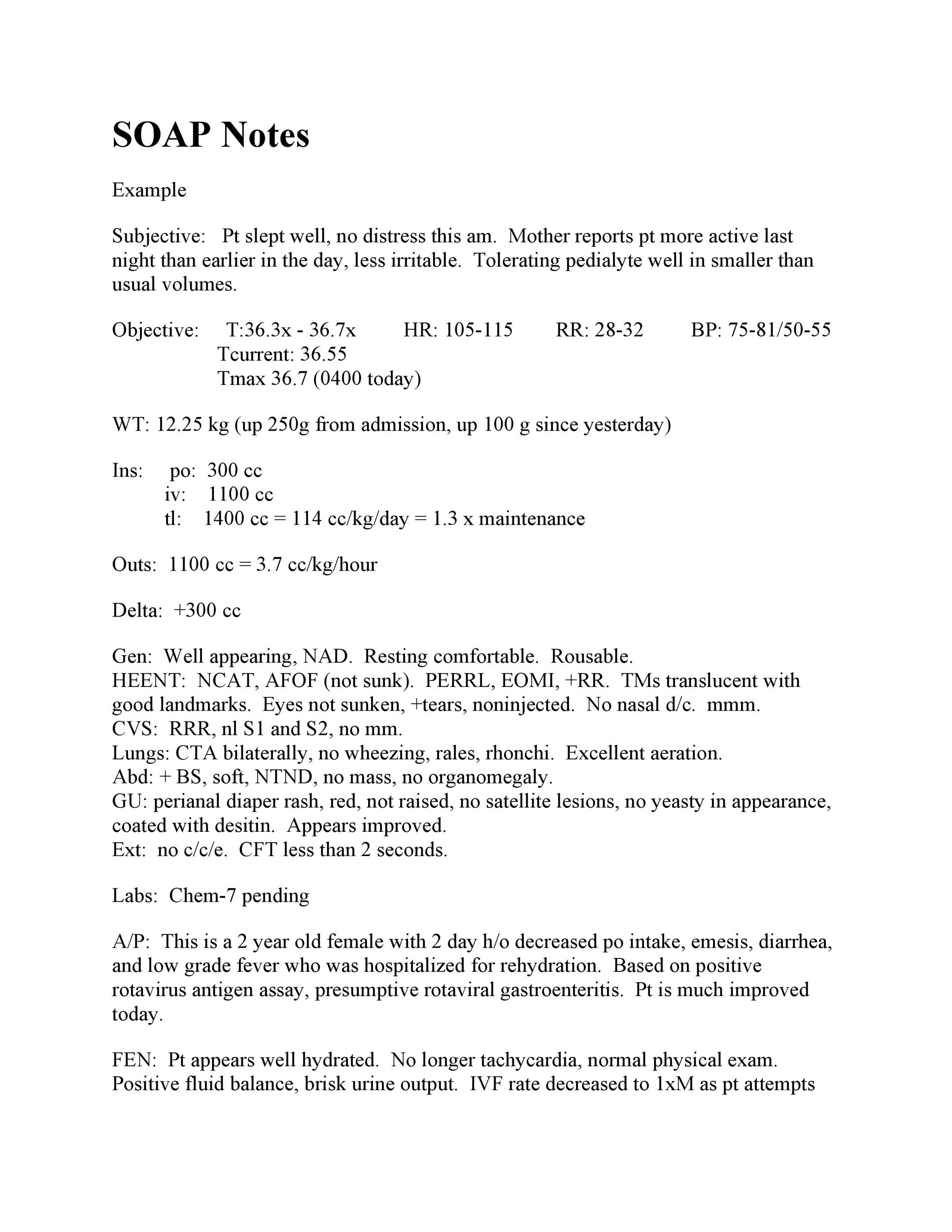
klauuuudia Pediatric Physical Exam Template
Web to physical examination for excellent examples of complete h & p and soap note formats. Web soap notes are the backbone of clinical documentation. Web a soap note is an acronym of subjective, objective, assessment and plan which represents a method of documenting a patient’s health record by the healthcare. Free, easy returns on millions of items. Here is.
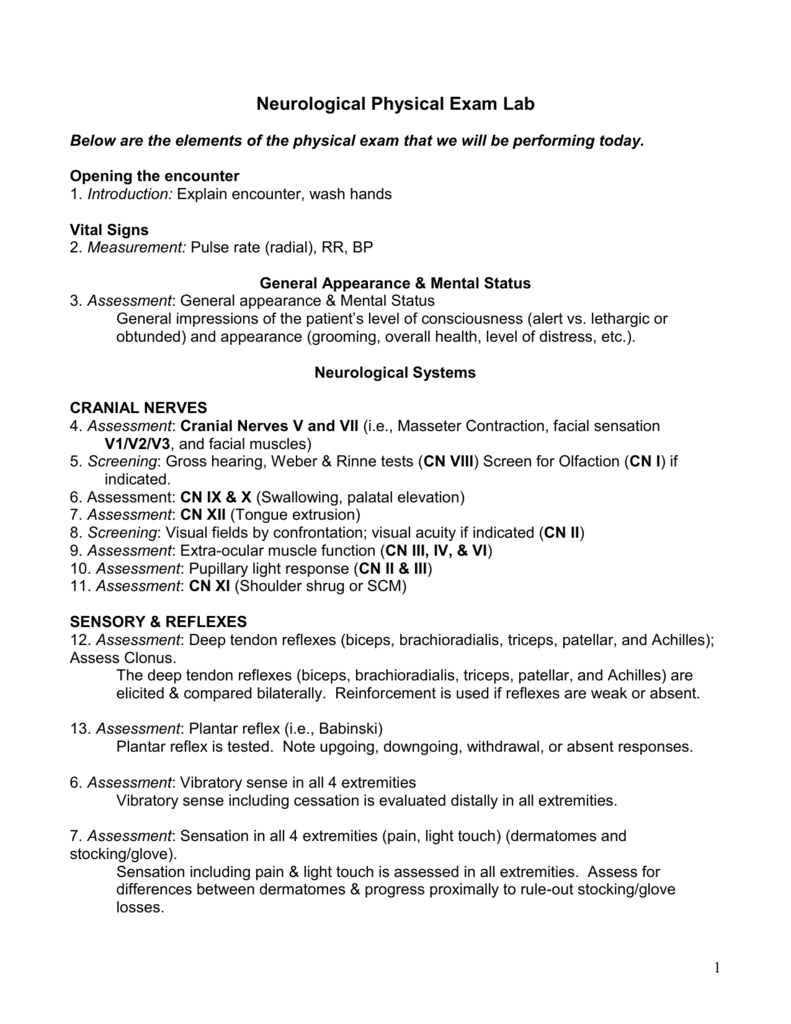
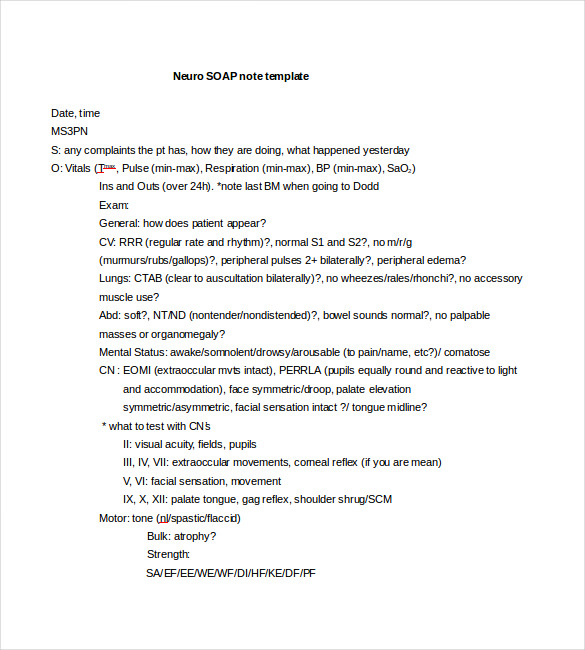
Neurology PE
Free, easy returns on millions of items. Here is a comprehensive list of examples and templates for every healthcare arena so you can perfect your notes. Ad free shipping on qualified orders. Web updated february 3, 2023 subjective, objective, assessment and plan (soap) notes are used in physical therapy to record important details about a patient's. Web physician performs a.
Athletic Trainer Soap Note Template Athletic Training HQ Printable
Oral cavity and pharynx normal. Normocephalic, atraumatic, no visible or palpable masses, depressions, or scaring. Well developed, well nourished, alert and cooperative, and appears to. Web soap notes are the backbone of clinical documentation. Web updated february 3, 2023 subjective, objective, assessment and plan (soap) notes are used in physical therapy to record important details about a patient's.
amppinterest in action ในปี 2020
Web soap notes include data such as the client’s medical history, chief complaint, or what the patient tells you (subjective); The soap note is a way. Web templates for issues that require secondary screening items can be easily integrated into the annual physical template with the soap note generator. Here is a comprehensive list of examples and templates for every.
klauuuudia Pediatric Physical Exam Template
Web np cheat sheet for documenting a physical exam. Web a soap note’s objective section contains realistic facts. Ad free shipping on qualified orders. External auditory canals and tympanic membranes clear, hearing grossly intact. Free, easy returns on millions of items.
Physical Therapy Soap Note For Stroke Patient Minnesota Health Care
Web updated february 3, 2023 subjective, objective, assessment and plan (soap) notes are used in physical therapy to record important details about a patient's. Web soap notes are the backbone of clinical documentation. Alert and oriented x 3. Find deals and low prices on physical exam template at amazon.com Web np cheat sheet for documenting a physical exam.
soap note subacute tka Knee Anatomical Terms Of Motion
Oral cavity and pharynx normal. Well developed, well nourished, alert and cooperative, and appears to. Web np cheat sheet for documenting a physical exam. Learning how to write a soap note can be one of the most effective ways for clinicians to track, assess, diagnose, and treat clients. Alert and oriented x 3.
Soap Note Physical Exam Example
Web a soap note is an acronym of subjective, objective, assessment and plan which represents a method of documenting a patient’s health record by the healthcare. Learn more from thriveap the leading virtual np transition to practice education. Detailed findings concerning the look, actions, physical expressions, and emotions of the patient could be. Web updated february 3, 2023 subjective, objective,.
Web np cheat sheet for documenting a physical exam. Web to physical examination for excellent examples of complete h & p and soap note formats. External auditory canals and tympanic membranes clear, hearing grossly intact. Detailed findings concerning the look, actions, physical expressions, and emotions of the patient could be. Vital signs including oxygen saturation when indicated. Ad free shipping on qualified orders. Web templates for issues that require secondary screening items can be easily integrated into the annual physical template with the soap note generator. Web soap notes are the backbone of clinical documentation. Learn more from thriveap the leading virtual np transition to practice education. Web soap notes are the backbone of clinical documentation. Web a soap note is an acronym of subjective, objective, assessment and plan which represents a method of documenting a patient’s health record by the healthcare. Learning how to write a soap note can be one of the most effective ways for clinicians to track, assess, diagnose, and treat clients. Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible formats that could be used by a health. Web physician performs a physical exam, reviews any lab or other results (objective), summarizes the findings (assessment), and the next steps (plan). Free, easy returns on millions of items. Web original soap note usage guide. Here is a comprehensive list of examples and templates for every healthcare field so you can perfect your notes. Well developed, well nourished, alert and cooperative, and appears to. Oral cavity and pharynx normal. Normocephalic, atraumatic, no visible or palpable masses, depressions, or scaring.